

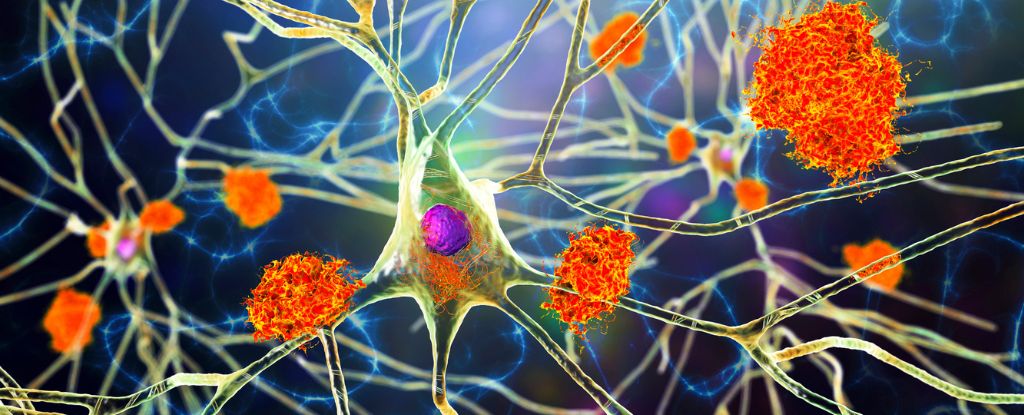
Twisted and tangled proteins are found in the brains of many of those who die with Alzheimer’s disease.
Some scientists suspect these neural knots can harm and even kill brain cells, but so far in clinical trials, drugs that have tried to target the tangles have shown limited success.
A promising new medicine has now been introduced by an international team, led by researchers at the University of Texas. The nasal spray can bypass the blood-brain barrier and blast tangles of tau proteins in living mice. The drug also works at clearing tangles from within and between human neurons in the lab.
The medicine was specially designed to recognize and destroy the most toxic form of tau proteins, like that seen in some cases of Alzheimer’s and dementia.
But that wasn’t the only challenge. Researchers also had to figure out how to get the medicine past the blood-brain barrier and into the brain’s cells.
Neuroscientist Sagar Gaikwad and his team decided to package the medicine into tiny bubbles that can slip past cell membranes. By spraying the medicine up the noses of mice, they were able to get around the blood-brain barrier.
In aged mice with tau-associated brain disease, a single spray was all that was needed to clear toxic tau from the brain. Two weeks later, the mice showed improved cognitive functions.
Of course, this does not mean the medicine will have the same impact on humans.
In a review of the findings for Science Translational Medicine, University of Edinburgh neuroscientists Soraya Meftah, Claire Durrant, and Tara Spires-Jones, who were not involved in the current study, note that while many tau-based therapies show promise in animal models, their translation into effective medicine for humans “has so far failed.”
Much more work needs to be done, but initial results from Gaikwad and his colleagues are hopeful.
In experiments on postmortem human brain tissue donated from patients with Alzheimer’s disease, dementia with Lewy bodies, and Pick’s disease (a form of frontotemporal dementia), the novel antibody medicine not only cleared away tau tangles but also stopped the release of ‘tau seeds’, which travel via connected neurons to tangle up proteins in other parts of the brain.
“Many open questions remain, including whether this treatment delivered intranasally in humans will allow penetration of the antibody in effective doses throughout our much larger brains and whether there are any potentially dangerous side effects like inflammation, which is a concern in all of the amyloid-directed immunotherapy trials,” write Meftah, Durrant, and Spires-Jones.
“Despite these limitations, this is an important piece of work.”
Gaikwad and his colleagues hope their technique inspires further research into the treatment of tau-associated diseases.
The study was published in Science Translational Medicine.