


Paxton Clarke, 13, sits upright in his bed as he yawns repeatedly and softly explains that he doesn’t remember an entire week of August.
While memories such as squeaking chairs come back to him in fragments, his mother, Jennifer Weatherbie, recalls every painful moment of how he dipped in and out of consciousness and nearly died.
She’s now seeking an apology from Nova Scotia Health and the Colchester East Hants Health Centre after Paxton was sent home by two doctors in Truro, only to end up in emergency brain surgery at the IWK Health Centre in Halifax.
“For them to basically tell us to leave with a child that can’t even walk or say more than a couple of words and is hallucinating … that’s not normal, in my opinion,” said Weatherbie.

Paxton Clarke’s mother took him to the Colchester East Hants Health Centre in Truro, N.S., on two occasions before he was diagnosed with a brain infection later that week in Halifax. (Dave Laughlin/CBC)
Paxton had been feeling poorly in July and the situation gradually worsened. At a walk-in clinic in Truro on Aug. 6, a doctor diagnosed Paxton with cluster migraines.
Weatherbie wasn’t convinced. She took her son to a crowded emergency department at the Colchester East Hants Health Centre on the following day, but left after two hours when people around her said they had already been there for nine hours or more.
Things escalated on Aug. 9. Paxton was unconscious and needed to be transported by ambulance to the emergency department in Truro. After seven hours, he was once again diagnosed with cluster migraines and told to rest at home.
As it turned out, Paxton had a strain of bacteria called streptococcus anginosus that developed into an infection and spread to his brain, according to Weatherbie. She said as soon as the IWK team saw her son’s MRI scans on Aug. 12, they immediately jumped into action.
“The doctors were standing there waiting for me and they were like, ‘It’s surgery or death,”” she said.
Worsening symptoms
Weatherbie’s gut instinct had prompted her to call the IWK after leaving the Truro hospital.
She said on top of the fact Paxton could barely walk or talk, he was vomiting, his forehead was protruding and his tongue was black and swollen. He also had a seizure seven hours earlier, which had never happened to him before.
“I carried him back out to the car, called the IWK and they said bring him straight down. He was in a CT scan under five minutes of being [there],” said Weatherbie.
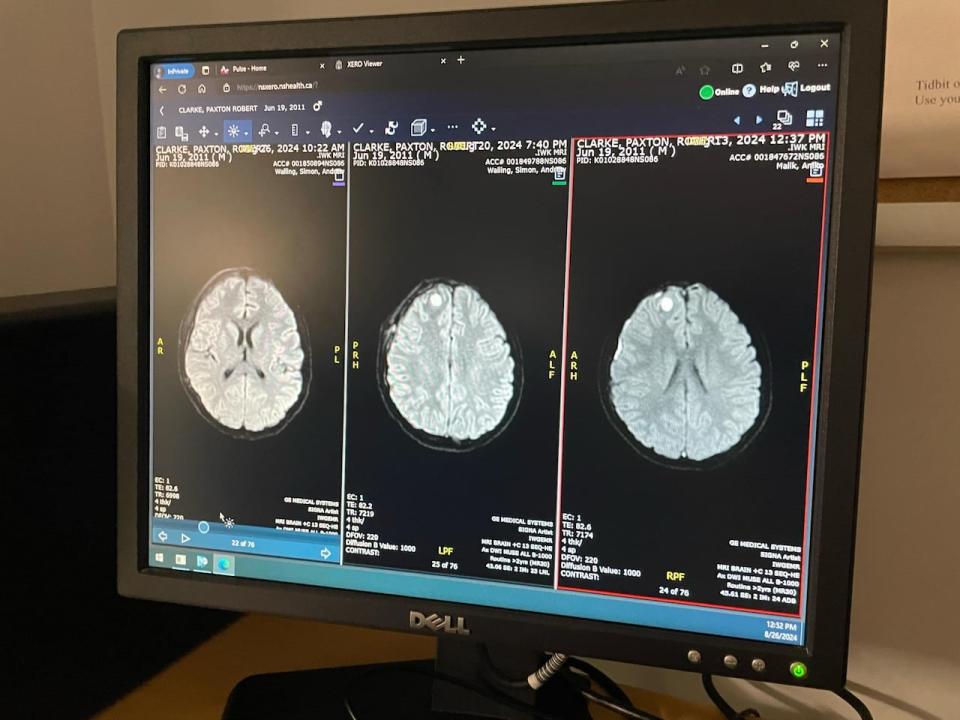
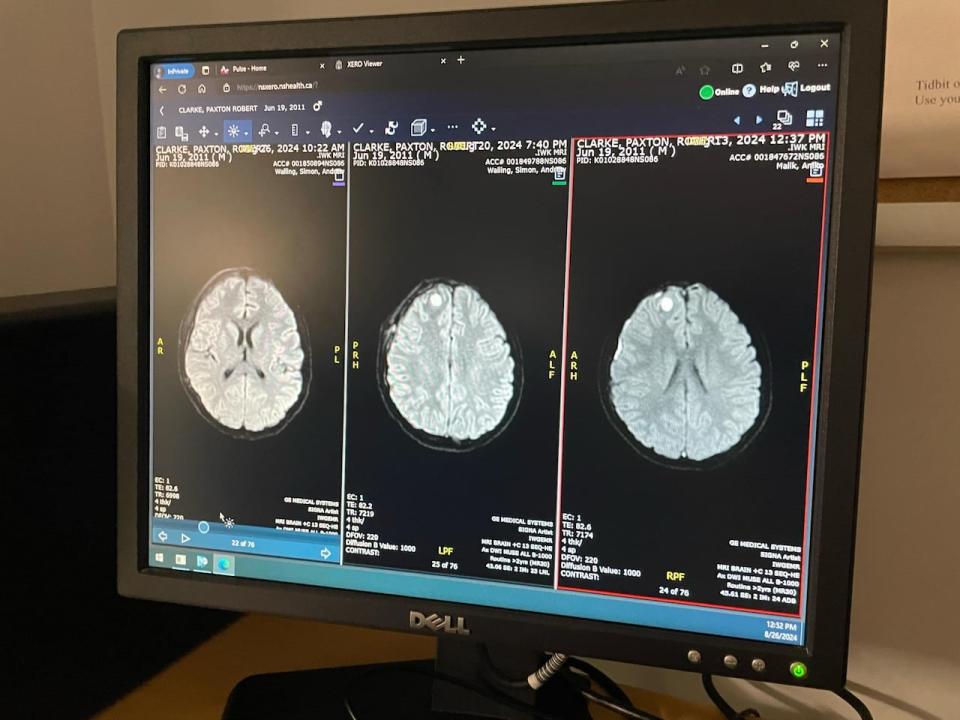
MRI scans of Paxton Clarke’s brain are shown on a computer screen at the IWK in Halifax. On the far right side, a white circle is the abscess at the height of infection, along with a glowing white line at the outer edge. The middle scan followed his first surgery, while the scan on the left was taken following his second surgery and shows the abscess is gone. (Jennifer Weatherbie)
She said a medical investigation was immediately launched by the IWK team over that weekend. She said her son had a chest X-ray in Truro, but no other scans. While Paxton had blood work done there, Weatherbie said she was told they would have to wait 24 hours for the results.
She doesn’t think his case was taken seriously in Truro, which is why she has filed a complaint with Nova Scotia Health.
“When you try and advocate for yourself and you’re not given what you’re asking for, that’s a problem,” said Weatherbie. “I get that doctors are smart, because they are, but you don’t live in that person’s body or you don’t live in their child’s body.”


Jennifer Weatherbie sought medical care for her 13-year-old son on four occasions during the second week of August. On the last visit, doctors at the IWK in Halifax diagnosed him with a brain infection that required emergency surgery. (Angela MacIvor/CBC)
Nova Scotia Health declined comment on this specific case.
“Any time there is a serious patient safety incident involving someone who has had contact with the health care system within Nova Scotia Health, a quality review is conducted,” spokesperson Jennifer Lewandowski said in a statement.
She said quality reviews are kept confidential, but Nova Scotia Health is committed to sharing any recommendations with family members.
Weatherbie also plans to file a complaint with the College of Physicians and Surgeons of Nova Scotia.
Patient safety concerns
Wendy Nicklin, a board member with Patients for Patient Safety Canada, said there are a “number of problems that are evident in this case,” starting with the need for Weatherbie’s tenacious advocacy.
“The other theme that’s quite evident here is diagnostic safety,” said Nicklin. “This is an example of delayed diagnosis and potentially the outcomes could have been even more grave.”


Wendy Nicklin, board member with Patients for Patient Safety Canada, says lessons should be learned from Paxton Clarke’s case. (Wendy Nicklin)
She said the “near-miss” is likely an indication of the current health-care crisis. Nicklin said while an internal hospital review is a good step, it’s not nearly enough. She said the case deserves a thorough debrief.
“The collective team involving the patient and family need to really walk through this and say, what can we change? What could be done better? And it’s not always more resources. It can be just a different process, a different way of handling something that can make a difference,” said Nicklin.
She said government officials also need to be included
“I think this incident involves several different locations and sites, interactions with professionals in different areas. And because of the health-system implications, I think there’s issues for government here too,” Nicklin said.
Road to recovery
Clarke is now home in Truro. Following a second surgery on Aug. 21, scans show the abscesses on his brain are reduced. He is continuing to get IV antibiotics with the help of home care.
Still, he has a long recovery ahead.
“He does know the seriousness of it,” said Weatherbie. “He’s had some good tears about death pretty much every day. And he’s frustrated because it’s just been a nightmare, but he’s getting a little better each day.”
MORE TOP STORIES